Sleep disorders in Australia continue to be a large and under-recognised problem. There are some 70 diagnosable sleep disorders, which contribute to a significant range of health and social problems. It is estimated that over 1.2 million Australians, or 6% of the population, experience a sleep disorder of some kind. In 2004, sleep disorders were associated with costs of $10.3 billion. The most common disorder is Obstructive Sleep Apnoea (OSA), and effects approximately 4% of the population in Australia.
For many people who suffer from snoring or Obstructive Sleep Apnoea (OSA), there are often funny stories about them missing their bus or train stop, falling asleep at the traffic lights, nodding off at the dinner table, being part of the conversation one minute and then fast asleep the next, or they “sound like a freight train”. These people are unfortunately the butt of family and friends jokes when in fact, excessive daytime sleepiness from snoring and OSA is a serious and potentially life threatening medical condition that has significant morbidity and mortality associated with it.
Neither snoring nor OSA should be interpreted as ‘just a nuisance sound’ and it can occur in ‘all age groups’ such as children, adults, and the elderly. Nor should the condition be associated only with the overweight or obese patients. Many people who are normal weight suffer from severe snoring or OSA. Epidemiological studies have shown that non-commercial drivers whom suffer from OSA have a two to seven times increased risk of road traffic accidents whilst other people have a marked increase in workplace accidents, sick days, and a shortened life expectancy.
Common signs and symptoms associated with OSA:
Apnoeas – periods where breathing stops.
Associated with ADD/ADHD in adults and children.
Choking or gasping while asleep.
Chronic Fatigue.
Depression.
Enuresis (bed wetting).
Excessive Daytime Sleepiness.
Heart attacks.
High blood pressure.
Lethargy.
Loss of libido.
Male impotence.
Marital and relationship problems.
Mood irritability.
Morning headaches.
Nocturnal reflux.
Personality changes.
Poor memory and concentration.
Snoring.
Sore dry throat on waking.
Waking with a feeling of choking or panic.
Weight gain.
Snoring and OSA is a serious and potentially life threatening medical condition
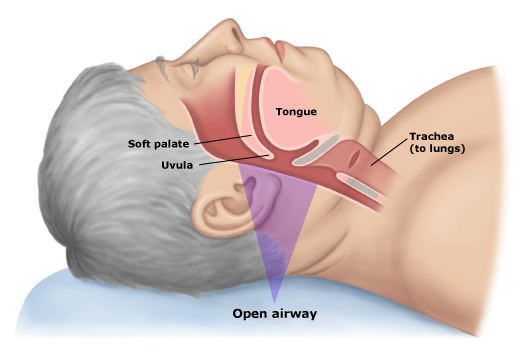
Normal Breathing
When you are awake, muscles in the throat and mouth hold the airway open and air passes quietly into and out of the lungs, typically through the nose. When you are asleep, these muscles relax but normally keep the airway open and allow respiration to continue quietly and unobstructed.
What is snoring?
It is a repetitive snorting or grunting sound that can be heard in a person’s breathing while asleep and is associated with respiratory air movement. When air cannot flow freely into or out of the throat past the flexible soft tissue structures of the tongue, soft palate, and uvula (the fleshy bit that dangles from the roof of your mouth) because of narrowing of the passages, or an inability to adequately breathe through the nose, vibration occurs as we breathe. This vibration is what we can hear when a person breathes and is called ‘Snoring’. The word “Hypopnoea” is used to describe a reduction in breathing that is shallower or slower than normal. Hypopnoeas are a common feature of snoring and result in a decrease in blood oxygen saturation levels that can occur many times per hour during sleep.
Causes of Snoring
• Excessive bulkiness of throat tissue
Children with enlarged adenoids and tonsils often snore, as do adults with large tonsils. Overweight people and those with large necks often snore as the excess neck tissue compresses the airway and lifts the tongue from the floor of the mouth.
• Alcohol and medications
When the throat tissues are too relaxed as a result of medications or drugs such as alcohol, benzodiazepines, sedatives, muscle relaxants, or others that cause sleepiness, the throat tissues can collapse in at the sides or the tongue can fall backwards and obstruct the airway.
• Long soft palate, long uvula, and constricted throat tissues
Many patients have anatomical variations in the structure of their throat tissues and have soft palates that are unusually longer than normal. The soft palate and uvula then hang further down the back of the throat and vibrate excessively when breathing. Other patients have constricted throat openings where the soft palate and tonsils are positioned causing a naturally occurring constriction at the junction of the soft palate and tongue which is easily obstructed during breathing whilst asleep. Many people also have a tongue that is larger than normal, or a lower jaw smaller than their tongue. A large tongue or loss of ‘tongue space’ can cause an increase in airway obstruction when asleep.
• Obstructed nasal passageways
A blocked or ‘stuffy’ nose requires extra effort to pull the air through it causing a type of vacuum in the throat that pulls the tissues of the throat together. Therefore, enlarged turbinates, a deviated septum, hay-fever, colds/flu, sinusitis, and allergies can all make snoring worse. In addition, when these conditions occur either temporarily or a nasal blockage is a permanent condition, the patient often needs to ‘mouth-breathe’. That in turn can make snoring worse as the lower jaw drops down and back during sleep.
• Edentulism
Complete tooth loss (edentulism) produces anatomical changes that may impair upper airway size and function such as loss of the vertical dimension of occlusion (loss of posterior teeth, worn dentures, or dentures not made to the correct bite thickness), reduction of the lower face height (the distance from the bottom of the nose to the chin is reduced) and mandible rotation (the lower jaw rests too close to the upper jaw). Recent studies have suggested that complete tooth loss favours upper airway obstruction during sleep due to a decrease in retropharyngeal (back of the throat) space. Therefore, it is considered that persons with old, worn, or incorrectly made dentures, or missing back teeth are at a higher risk of snoring and OSA
• Upper Airway Resistance Syndrome
The term upper airway resistance syndrome (UARS) was coined to describe a group of patients who did not meet the criteria for diagnosis of obstructive apnoea-hypopnea syndrome and thus were left untreated. UARS is a clinical syndrome of sleepiness resulting from respiratory effort-related arousals, but without obvious apnoeas, reductions in airflow, or drops in blood oxygen saturation levels. This results in fragmented (very broken) sleep patterns and increased daytime sleepiness or fatigue. These patients are often misdiagnosed on sleep study due to these absent findings. UARS was first recognised in children in 1982, but the term UARS however, was not used until adult cases were reported in 1993. Controversies do exist regarding UARS as some clinicians have rejected or doubted its existence as a distinct clinical entity and rather consider it to be part of the sleep disordered breathing that includes snoring, OSA, obstructive hypopnoea syndrome, and hypoventilation (shallow breathing). Diagnosis relies on the finding of increasing airway pressure during sleep associated with temporary arousals as seen on EEG, and an abnormal blood pressure response.
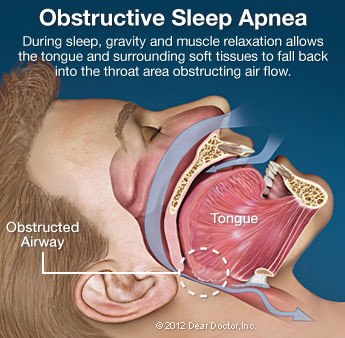
What is Obstructive Sleep Apnoea?
The word “apnoea” is used to describe the complete absence of breathing for more than 10 seconds at a time that usually occurs during sleep. The forms of apnoea can be:
Central – where there is no effort made to breathe.
Obstructive – despite repeated efforts to breathe, air cannot pass into the lungs because of a blockage.
Mixed – is a combination of Central and Obstructive apnoea.
Unlike snoring where air movement into and out of the lungs occurs but is restricted or lowered, Obstructive Sleep Apnoea (OSA) is when no air movement can occur because of an obstruction in the throat or air passages. When an obstruction occurs and fresh air no longer passes into the lungs, it is reduced, or is absent for more than a few seconds, defense mechanisms in the body are alerted. As blood oxygen levels fall, the brain sends signals to ‘wake the body up’ and turn on muscles of the throat to return them to a less relaxed state so that breathing can recommence. Often this arousal is accompanied by snoring sounds, or a choking / gasping sound. Although sufferers may not recall waking up from sleep, the normal sleep pattern is disrupted and is called a ‘ respiratory arousal’.
In severe cases of OSA, people can experience a respiratory arousal from their sleep up to several hundred times each night, yet arousal to full wakefulness rarely occurs so few, if any of the events during the night can be remembered by the person the next day, but results in severely fragmented sleep patterns and chronic daytime tiredness. People with snoring and sleep apnoea conditions regularly report headaches and a feeling of being ‘hung over’ on waking in the morning.
The severity of sleep apnoea depends on how often breathing is interrupted, and is scored on a sleep study as an AHI (Apnoea / Hypopnea Index) and the following averages can be used as a guide:
Normal – less than 5 per hour.
Mild – 5 to 15 per hour.
Moderate – 15 to 30 per hour.
Severe – More than 30 per hour.