All questions people have regarding their planned oral surgery procedure are always addressed during the consultation appointment. Dr Eldridge strives to inform his patients as best and as much as possible regarding the procedure itself, what happens before the appointment, and any post operative instructions. However, below are some of the most commonly asked questions regarding oral surgery.
ORAL SURGERY
1. How long will I be off work or school?
Everybody heals differently and handles stress to the body in a different way, and it depends very much on what type of surgery is being performed. Most people recovery quickly and just need to rest for 24 hours. A sick certificate for school or work is always provided when necessary. The following are some guidelines on the ‘average’ time we allow.
2. What kinds of foods can I eat?
It’s all about how you feel and what type of surgery was performed. For simple extractions, typically a soft diet for 24 – 48, but in general almost all foods are able to be eaten post operatively. For multiple extractions and wisdom teeth surgery, a soft diet of soup and food that does not require much chewing for 2 – 3 days, then foods such as pasta and fish up to day 5 – 6 and then from day 7 typically a normal diet can be consumed.
3. How much will it cost to get my teeth out?
Please see our Pricing Structure page. All costs are discussed in full with a complete range of options provided during the consultation appointment.
4. What’s involved in a consultation? Do I really need one?
A consultation is always done prior to any surgery being conducted. This consultation is extremely important for both yourself and Dr Eldridge, and is performed in a non-threatening office environment to discuss all of your treatment goals, concerns, medical and dental history, medications. In addition, if we require further Xrays, blood tests, or further information, then this is arranged during the consult. We are then able to provide you with a full range of options to allow you to make an informed decision. This process also helps take away a great deal of anxiety from the planned procedure.
5. Will I be really swollen?
With any surgery, some minor swelling and discomfort is considered normal. However, there is absolutely no reason why anything more than this should occur. We provide pre, during, and post operative medications and use techniques to keep swelling and discomfort to an absolute minimum where possible. It is also very important that you take the anti-swelling and pain medication that is prescribed to you exactly as instructed.
6. When can I resume physical activity?
Depending on the surgery performed, most people can return to normal activity within 24 hours. Major surgery will require more rest and it is usually recommended that people allow for 5 – 7 days off work at a reduced capacity. If you are a competitive athlete, then it may take 7 – 12 days to feel completely normal, especially if you have had a general anaesthetic. Recovery from IV sedation however is much quicker.
7. How long will it take to have my wisdom teeth removed?
For a simple extraction, it usually only takes several minutes (if not less) by an experienced practitioner. Typically for four wisdom teeth it takes no longer than 35 – 45 minutes. When having wisdom teeth removed in the chair we always allow 1 hour from start to finish including recovery time. Oral surgery should never be rushed so it is as relaxing as possible for everyone concerned. However, oral surgery including implants, extractions, and wisdom tooth removal should never take exorbitant amounts of time. Whilst complications can and do occur, if an extraction is taking longer than 30 minutes, something is not going to plan.
Below is typically what to expect after having your wisdom teeth removed:
– Hours to 1 Day
• Slow bleeding or oozing that can be controlled by biting on the gauze packs you have been given, or a clean piece of cloth (such as a hanky) for 20 minutes at a time.
• Mild swelling and pain of the extraction sites.
– 1 to 7 Days
• Mild swelling and discomfort of the extraction sites.
• Small amounts of bruising can occur around the cheeks, jaw, and neck.
• The need to eat a soft diet where the amount of chewing is minimised.
• Discomfort, pain, and restricted mouth opening begin to improve by Day 3 – 4.
IMPLANTS
1. Who is suitable to dental implants?
Most people that are generally healthy and have sufficient bone levels are good candidates for implants. If there is insufficient bone, then further procedures may be required to add bone to the area of the implant. This is all determined during the consultation and xray stage.
2. Will I be able to eat properly with an implant?
Once completed, an implant will function just like a natural tooth and all foods will be able to be eaten without concern.
3. Can implants be placed immediately after tooth extraction?
In most cases yes they can be placed into an extraction site during the same appointment as long as there is sufficient bone levels and no infection present. Each case is assessed individually as there are a number of factors that determine if immediate implant placement is possible.
4. How long will my implant last?
All going well, there is no reason why an implant will not last a lifetime. It is important however that regular dental checkups and oral maintenance with your general dentist occurs. Like all things to do with the body, implants can fail for a number of reasons such as gum infections, bruxism, trauma, and general medical illness and disease.
5. Can my existing denture be used to attach to implants?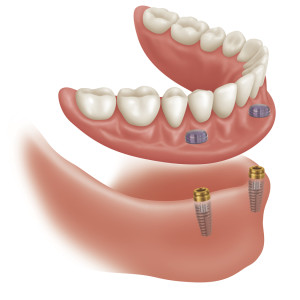
If the denture is in good condition and does not require replacement any time soon, then there is no reason why it cannot be modified to fit the new implants. This saves considerable costs by not having to have new dentures constructed.
6. Are there any risks involved with having implants?
Like any surgical procedure, complications can and do happen but are quite rare in most cases. Damage to nerves and blood vessels can happen if the implant is placed in the wrong position, or too deep into the bone structures. These risks however are minimised with good pre-surgical planning and the use of CT scans and xrays before surgery starts.
7. What happens if my implant fails?
The risk of implant failure is quite low. In fact up to 97% of implants placed are successful. If an implant fails it is typically during the ‘osseointegration’ phase where the body rejects the implant or it becomes infected. If this occurs the implant is usually removed and after a suitable healing phase, a new implant is placed which in most cases is successful.
8. What are the stages of implant placement?
We work with the general dentist in most cases that follows the following steps:
– Diagnosis and evaluation.
– Treatment planning.
– Surgery which may be extraction, bone grafting, implant placement or a combination of all 3.
– Healing phase that may be 3 – 6 months. A healing cap or tissue former is placed during this period to shape the gum prior to a crown being constructed by the general dentist.
The general dentist now takes over the remainder of the work that includes impression taking, restoration of the crown, and implant / oral hygiene maintenance.
For patients with special needs or dental phobias that require an extra level of care, the entire procedure from start to finish is conducted through our practice.
9. How much does an implant cost?
At the Hobart Orofacial Pain and Special Needs Clinic our mantra is to make implants as affordable as possible for as many people as possible. They are still an expensive treatment option for many people however once the crown is placed by the general dentist. Please see Our Pricing Structure page for a breakdown on the most commonly used item numbers for implant placement.
10. Do I need a referral to attend your practice for Oral Surgery or Implant treatment?
No. All new patients are very welcome at all times. We will require an up-to-date medical and medication history however, that we can easily obtain from your current GP. A medical history form will also be provided to you on the day of your appointment to allow us to make sure we have the most current information on your health as possible. We will also keep in touch via written correspondence with your regular dentist and GP before and after and treatment is completed.

